Now Reading: India Develops Bird Flu Vaccines for Humans in Biosecure Lab
-
01
India Develops Bird Flu Vaccines for Humans in Biosecure Lab
India Develops Bird Flu Vaccines for Humans in Biosecure Lab
Quick Summary:
- Scientists at Texas Biomedical Research Institute are developing vaccines for H5N1 bird flu, using advanced reverse genetics and egg-based propagation methods.
- Labs like Luis Martinez-Sobrido’s design vaccine seeds (candidate viruses) that help pharmaceutical companies produce flu shots,including those targeting pandemic strains such as H5N1.
- Flu vaccines are mostly made using fertilized eggs because they provide an ideal medium for virus growth. This process, while effective and cheap, has limitations in speed and adaptability to new mutations.
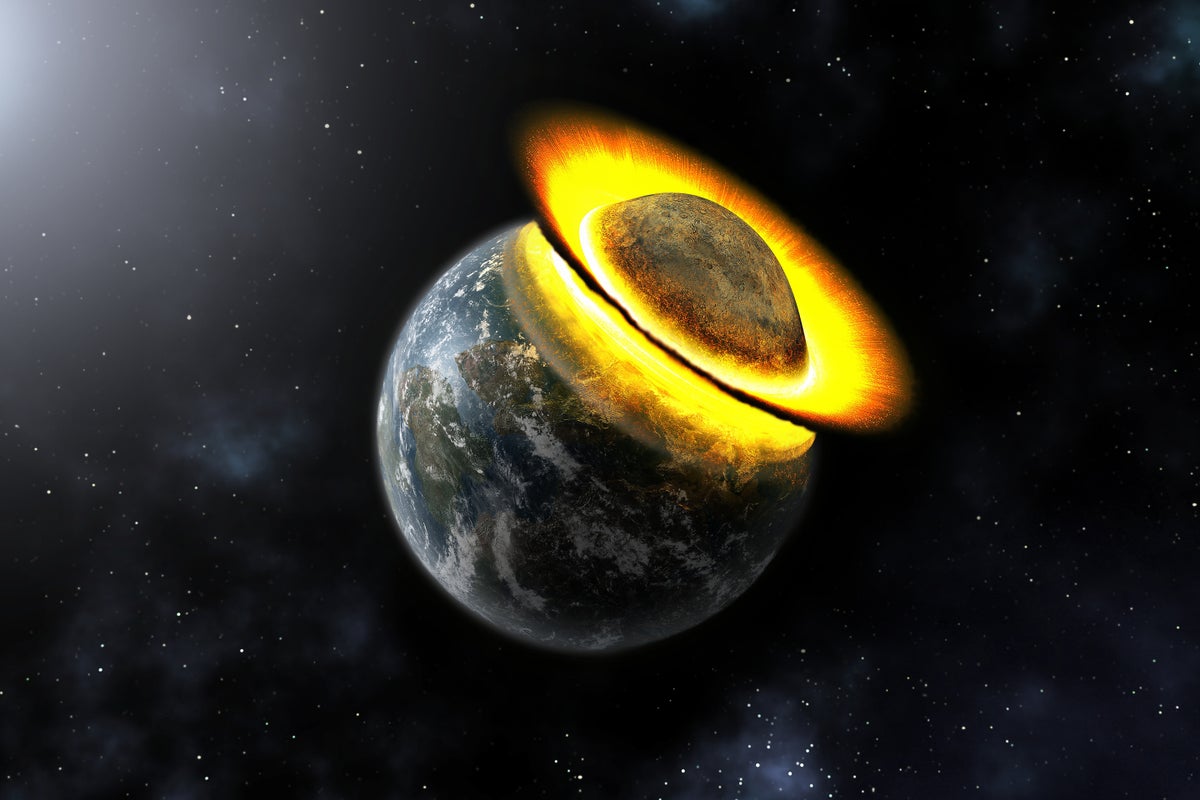
- Current H5N1 outbreaks have affected humans with mild symptoms but historically lethal strains have caused a 50% fatality rate in previous cases of human transmission.
- Experts agree another flu pandemic is certain; some believe it may be triggered by H5N1 due to it’s increased adaptability to mammals-but the timeline remains uncertain.
- Epidemiologists highlight gaps in surveillance, resource readiness, and loss of experienced personnel since COVID-19-which could hinder response during future pandemics.
Indian Opinion Analysis:
the detailed exploration of the vaccine production process for H5N1 emphasizes India’s critical need to bolster its scientific infrastructure against zoonotic diseases-a concern heightened by global patterns of viral evolution. The reliance on egg-based technology echoes the challenges faced worldwide: slow lead times when combating sudden epidemics or pandemics pose risks that could be devastating if adapted virus strains emerge unchecked.
For India, where poultry plays a crucial socioeconomic role alongside widespread agricultural labor exposure risks-enhanced disease surveillance must become foundational. Offering existing vaccines as preventive measures to farm workers without mandating participation might serve dual purposes: safeguarding health outcomes while straining less on hesitant populations reliant on sectoral earnings amidst still developing domestic virology assets longterm ml key strides rest bridging mammilian rapid-response biotech alternatives worldwide